1) Welcome to a #tweetorial on what every #ICU #nurse should know about #hypertensive crisis, or #hypertensive #emergency as it is now more properly termed. I’m Bryan Boling @bryanboling, ICU #NP, & co-host of the @icuscenarios podcast. Follow this 🧵for 🆓CE/#CME credit!
2) This accredited educational activity is intended for healthcare providers & is supported by grants from AstraZeneca, Bayer, & Chiesi. Faculty disclosures https://cardiometabolic-ce.com/disclosures/. Like ❤️this topic? More CE/#CME on #hypertension mgt at https://cardiometabolic-ce.com/category/hypertensive/.
3) So let's start with a case: 65yo ♂️, presents to the #ED with #headache, lethargy & confusion. PMH: #HTN, #hyperlipidemia, #DM2, COPD. Initial VS: HR 85, BP 205/120, T 37.2 RR 12, SpO2 92% on RA. Family reports that he has been more lethargic over the past 2 days.
5) CTH reveals no acute intracranial hemorrhage. Family states that he is Rx'd lisinopril for HTN, but is not good about taking it as prescribed. Is this hypertensive emergency?
— cardio-met (@cardiomet_CE) May 3, 2022
a) Yes, SBP > 200
b) No, SBP not > 220
c) Yes, HTN+organ damage
d) Need to know his baseline to say
6) YES! Yes, this is a #HTN #emergency. Contrary to popular misconceptions, there is no numerical BP that "defines" HTN emergency. A HTN emergency is substantially elevated BP accompanied by hypertension-mediated organ damage (HMOD), so the correct answer is C.
7) Another "practical" definition of hypertensive emergency, which separates it from hypertensive "urgency," is that parenteral #antihyperternsives are required to bring it under control and address that end-organ damage.
8) End-organs include kidney🫘, brain🧠, retina👁️, heart🫀, & large arteries. As the name implies, HTN emergencies are time-sensitive & need rapid intervention in order to preserve end-organ function.
9) There are multiple possible presentations of HTN emergencies, but the most common are malignant hypertension, hypertensive #encephalopathy, and hypertensive thrombotic microangiopathy. See 🔓
10) Other possible presentations are associated with #cerebral #hemorrhage, acute #stroke, acute coronary syndrome #ACS, cardiogenic pulmonary edema, aortic aneurysm/dissection, & severe preeclampsia and eclampsia.
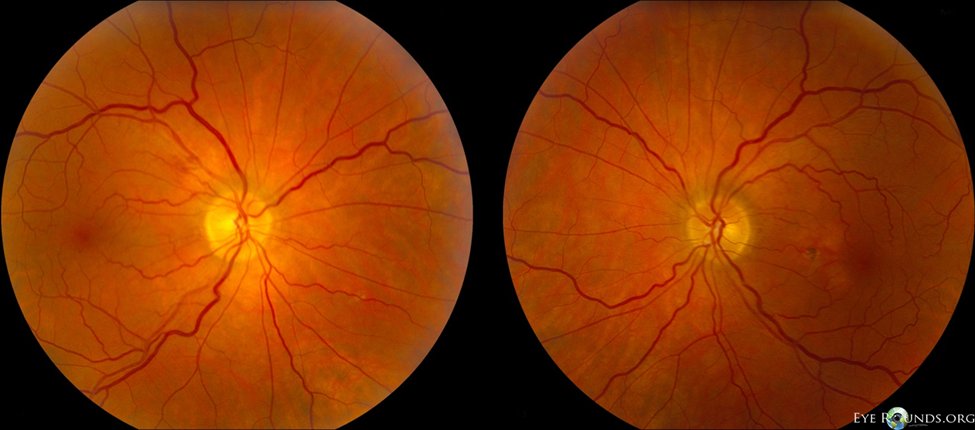
11) Malignant hypertension comes on rapidly and is associated with extremely elevated #BP (>200/120). It is commonly associated with bilateral retinopathy, with #papilledema being frequently present.
12) Patients w/hypertensive #encephalopathy may present with a number of neurological symptoms including lethargy, #seizures, cortical blindness, even #coma. It is important to R/O other causes of these symptoms, such as acute ischemic #stroke or intracerebral hemorrhage #ICH.
13) In hypertensive thrombotic microangiopathy, patients develop #hemolysis and #thrombocytopenia related to the #HTN. As with hypertensive encephalopathy, it’s important to rule out other potential causes of these findings.
15) IV beta blockers like labetalol are a great option for reducing BP in the acute setting. What other drug do you most commonly give in hypertensive emergencies?
— cardio-met (@cardiomet_CE) May 3, 2022
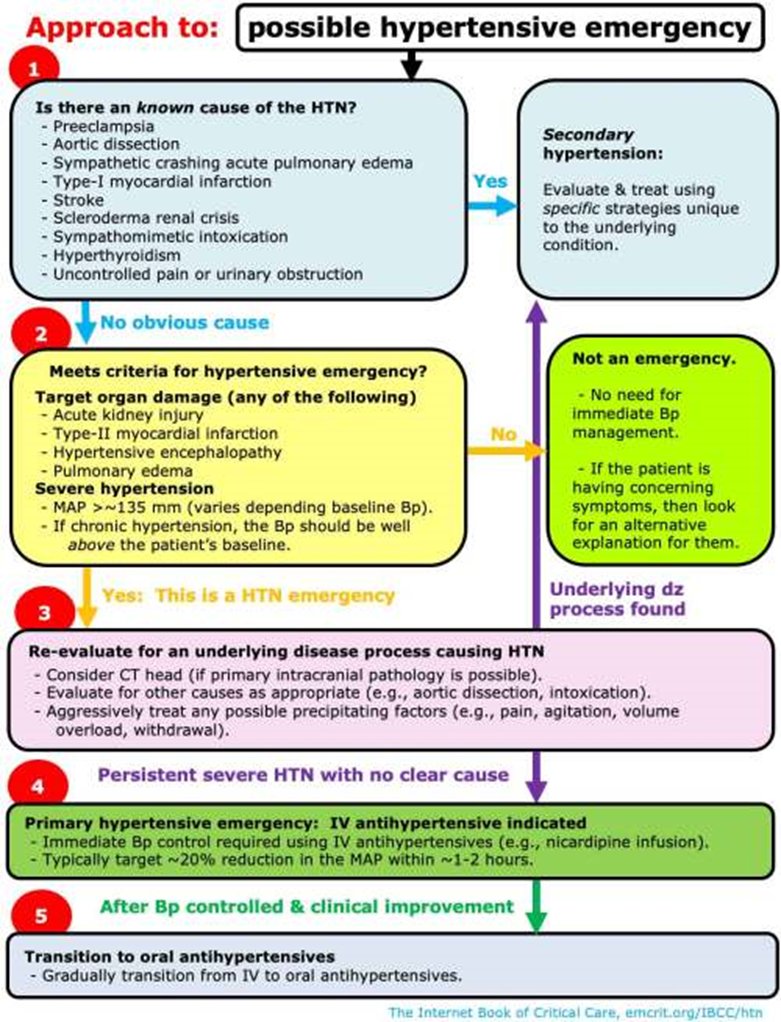
16) Check out the results of the poll to see what your fellow #nurses & other #ICU clinicians are seeing in use. And check out this busy but comprehensive flow chart for GETTING TO the therapeutic decision from 🔓
17) All of the choices in tweet 15 would be appropriate, but most commonly in hypertensive emergencies, a continuous infusion is preferred over IVP dosing. It’s important for nurses to understand how to titrate the gtt they’re using including how frequently to adjust the rate.
18) Altho #nitroprusside is sometimes used in cases of extreme hypertension, its downsides make it less than ideal except in specific circumstances (acute cardiogenic pulmonary edema & aortic disease) & it can ➡️reflex tachycardia, so should be given w/a beta-blocker.
19) The mainstay drugs for BP control in hypertensive emergencies are labetalol IVP & nicardipine gtts. Esmolol is rapidly titratable beta-blocker that can be given as a continuous infusion. Clevidipine may be the best choice, but it’s not universally available (yet).
20) We'll discuss each of these options when we return TOMORROW! See you then–your CE credit is waiting!
👏@TheBlondeRN @GoodishIntent @NursePatMacRN @reepRN @concernecus @VietHeartPA @Lross246 @critconcepts @Nursing_Heretic @shesinscrubs @MomRobe @thanksgoose @MitchAbreuEllis
21) Welcome back! I am #ICU #nurse @bryanboling and you are earning CE/#CME while we talk about the mgt of #hypertensive #emergencies. Shout outs to @josephcmanning @HeartRhythmNP @NurseTexas1 @NurseNoodles1 @CaitlintLohuis @GooseCG @Sydney4Real @Ejost244 @nypac
22) So back to those options: Labetalol IVP is rec'd as 1st line in guidelines, but often is insufficient to really control ⬆️⬆️hypertension. Esmolol is a beta-blocker option administered as a gtt. But it generally doesn’t work much better & gives your pt quite a bit of volume.
23) #Nicardipine is a calcium channel blocker that is the real workhorse for acute BP lowering in most hospitals.
24) To titrate, start at 5mg/hr & ⬆️ by increments of 2.5 to a max of 15. Nicardipine has a longish half-life, so it’s not rapidly titratable. Wait 15-30 mins before increasing. Once the BP reaches target, ⬇️the dose slightly to avoid overshooting and inducing hypotension.
25) Besides the sluggish titration response, nicardipine tends to be somewhat dilute and therefore gives your patient a little more volume than may be desirable.
26) #Clevidipine is also a CCB, but w/ a much shorter half-life, making it truly titratable and good for rapid, tight control of #BP. It’s better at BP control than nitroprusside & better at maintaining tight control of BP than nicardipine (🔓https://pubmed.ncbi.nlm.nih.gov/18806012/).
27) Start at 1-2mg/hr & double every 2 mins. As you get close to the target BP, slow titration to every 5-10 mins & increase slowly. The risk of overshooting & causing hypotension is lower than with nicardipine because of the short half-life. The normal dose range is 1-32 mg/hr.
28) Caution: Usually, the only lipid-emulsion infusing in our patients is propofol. Having a 2nd white infusion can be confusing, so ensure that both lines are clearly labeled to avoid errors. Consider using opposite arms if propofol & clevidipine are infusing simultaneously.

29) Clevidipine may not be available in all hospitals due to cost or other formulary factors. If not available, nicardipine is probably the second best option for controlling BP in hypertensive emergencies.
So back to our case.
30) Our patient was given bolus doses of IV labetalol, but that did not adequately reduce BP. A clevidipine gtt was started and we were able to achieve goal BP. Our patient is in the ICU 24h later.
31) Clevidipine has been infusing at a stable dose for the past 12h with good control of the BP. You get an order to start scheduled oral labetalol. Should you turn off the clevidipine drip before giving the labetalol? Answer before you scroll ⤵️!
32) The correct answer is no. The half-life of clevidipine is extremely short, ~1 minute, & most patients will see a return to their previous BP within 5-15 min of discontinuation unless the cause of HTN is reversed (in cases of secondary HTN) or another agent has taken effect.
33) In this case, the oral labetalol will need to achieve its steady state before discontinuing the clevidipine so that we don’t see an⬆️in the BP. Expect to continue the clevidipine gtt, titrating the dose ⬇️to keep the BP in goal range, until the labetalol takes full effect.
34) Because of the short half-life, there is little worry about hypotension, as clevidipine can be down-titrated rapidly or even stopped if BP begins to fall.
35) You are able to wean the clevidipine off once the labetalol has taken effect and the patient’s blood pressure is now well controlled on oral agents. His confusion and blurry vision have resolved and he is ready to be downgraded from the ICU.
36) Hey, you do great work! And now you can claim your free 0.5h CE/#CME credits, go to https://cardiometabolic-ce.com/htn4/. I’m @bryanboling. Follow @cardiomet_CE for more tweetorials and visit us at http://www.cardiometabolic-ce.com! #medtwitter #cardiotwitter #nursetwitter #FOAMed
37) Special shout-outs to @icuscenarios, @CritCareNotes, @UKAPPFellowship, and @PocusGeorgetown!
Hey everybody–follow @ckd_ce too! More education-by-tweetorial and expert authors!
Originally tweeted by cardio-met (@cardiomet_CE) on May 3, 2022.
